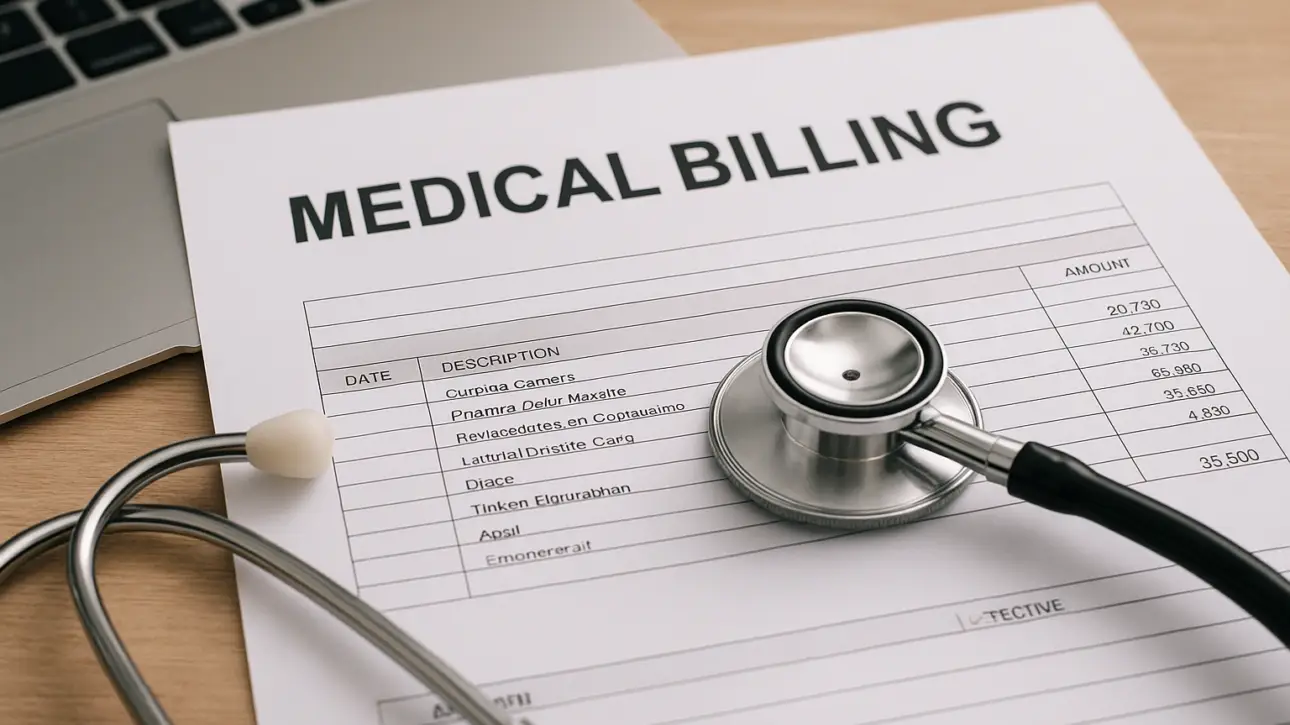
A superbill is one of the most essential documents in the medical billing process. It captures every detail of a patient’s visit, from the provider’s information and diagnosis codes to the procedures performed and payment details. When completed accurately, a superbill helps billing teams create clean, error-free claims that lead to faster reimbursements.
For healthcare…