A superbill is one of the most essential documents in the medical billing process. It captures every detail of a patient’s visit, from the provider’s information and diagnosis codes to the procedures performed and payment details. When completed accurately, a superbill helps billing teams create clean, error-free claims that lead to faster reimbursements.
For healthcare practices aiming to improve financial accuracy, understanding how superbills work can reduce denials and streamline revenue cycles. Let’s explore what a superbill includes and how it fits into the modern billing workflow.
Table of contents
What Exactly Is a Superbill?
A superbill is a comprehensive, itemized document that healthcare providers use to summarize the services they deliver during a patient visit. It serves as the link between patient care and insurance billing, ensuring all details are correctly recorded before claims are submitted.
Unlike a standard invoice, a superbill contains crucial coding data such as CPT (Current Procedural Terminology) and ICD-10 (diagnosis) codes, along with provider details and service dates. When accurate, this document helps billers submit clean claims, minimize payer rejections, and maintain compliance across payers and insurance networks.
Key Components of a Superbill
A well-structured superbill ensures accuracy and transparency between healthcare providers, billing teams, and payers. Each section of the document plays a crucial role in crafting a clear claim that leads to faster reimbursement and fewer denials. Let’s look at the main components one by one.
Patient and Provider Information
Every superbill starts with essential identifying details.
It includes the patient’s full name, date of birth, address, and insurance policy number, along with the provider’s name, NPI (National Provider Identifier), and practice address.
✅ Example:
Patient: Sarah Collins, DOB: 02/15/1985
Provider: Dr. John Smith, NPI: 1245678901, Sunshine Family Clinic
Accurate data here prevents claim rejections caused by mismatched or missing information.
Procedure (CPT) and Diagnosis (ICD-10) Codes
These codes form the core of a superbill. CPT codes represent the medical procedures performed, while ICD-10 codes identify the patient’s diagnosis or condition. Pairing the right CPT and ICD-10 codes ensures medical necessity and proper reimbursement.
✅ Example:
CPT: 99213 – Office or outpatient visit, established patient
ICD-10: J06.9 – Acute upper respiratory infection, unspecified
If these codes don’t align correctly, the payer may deny or delay the claim, a common issue our Medical Coding Services help prevent.
Date of Service and Provider Signature
The date of service confirms when care was delivered, and the provider’s signature validates that all information listed is accurate. This step is not only required by payers but also crucial for compliance and record-keeping.
✅ Example:
Date of Service: 10/05/2025
Signature: Dr. John Smith, MD
Even a missing signature can delay reimbursement or trigger an audit request.
Additional Notes and Modifiers
Some claims require modifiers or special notes to clarify unique billing situations. Such as multiple procedures, bilateral services, or exceptional circumstances. These notes help billers and payers understand the context of care.
✅ Example:
Modifier -59 may indicate a distinct procedural service performed on the same day.
Clear documentation in this section reduces follow-ups and supports smoother claims processing.
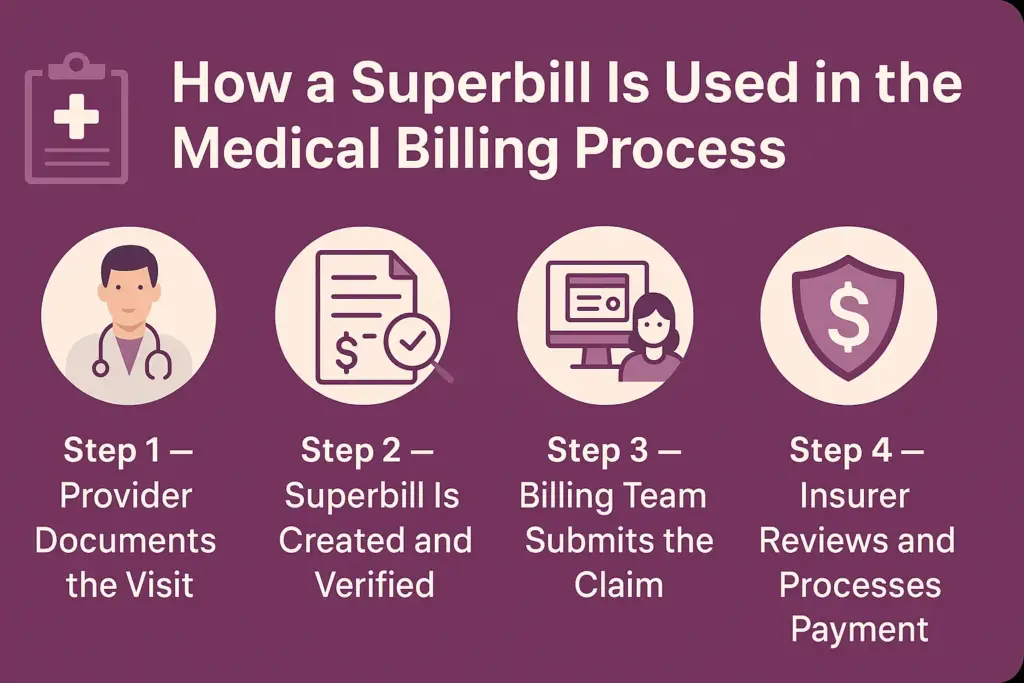
How a Superbill Is Used in the Medical Billing Process
A superbill acts as the bridge between patient care and payment collection. Once a patient visit is completed, this document guides the billing team through every stage, from capturing encounter details to claim submission and reimbursement. Here’s how the process typically unfolds:
Step 1 — Provider Documents the Visit
The process starts when the healthcare provider records the patient encounter. During the visit, the provider notes the diagnosis, procedures performed, and any additional medical observations. These details form the foundation for accurate CPT and ICD-10 coding.
✅ Example: A physician diagnoses strep throat (ICD-10 J02.0) and prescribes antibiotics — both actions are noted in the visit documentation.
This ensures that every clinical action can be correctly billed later.
Step 2 — Superbill Is Created and Verified
Next, the provider or front-office staff creates the superbill using the documented details. The superbill is then verified by the billing or coding team to ensure all patient, provider, and coding data are accurate and compliant.
Verification prevents costly mistakes — such as mismatched codes or missing insurance information — that could delay payment.
At this stage, many practices choose to work with professional teams like our Medical Billing Services to ensure accuracy, compliance, and faster turnaround.
Step 3 — Billing Team Submits the Claim
Once verified, the superbill is converted into a claim using a billing system or clearinghouse. The billing team ensures all payer requirements are met before submission.
Claims are typically sent electronically to insurance companies through HIPAA-compliant platforms. This step is where automation and expertise come together to avoid denials.
Step 4 — Insurer Reviews and Processes Payment
The insurance company then reviews the submitted claim. If everything aligns — patient coverage, codes, and documentation — the claim gets approved and reimbursed. If there are discrepancies, the payer might request clarification or issue a denial, requiring resubmission.
After payment, the billing team reconciles the claim and posts the payment to the patient’s account.
✅ Result: A clean and complete superbill ensures smooth claim flow and faster payments with minimal errors.
Why Accuracy in Superbills Matters
Accuracy in superbills is crucial for smooth claim submission and timely reimbursements. Even minor errors, like missing modifiers, incorrect CPT codes, or incomplete patient details can cause claim denials, payment delays, or compliance issues.
When a superbill is inaccurate, the billing team must spend additional time correcting and resubmitting claims, increasing administrative workload and reducing revenue efficiency.
This is why many healthcare providers rely on professional Medical Coding Services to ensure every CPT and ICD-10 code is applied correctly and fully compliant with payer and federal guidelines. Expert coders understand documentation standards, helping prevent rejected or underpaid claims.
For official coding references and updates, providers can always refer to resources from CMS or the AAPC for accurate, up-to-date compliance guidance.
Common Errors in Superbills and How to Avoid Them
Even experienced providers can make mistakes in superbill documentation. Recognizing common pitfalls and knowing how to prevent them helps maintain billing accuracy and ensures a clean claim rate.
Missing Codes or Wrong Modifiers
A missing CPT or ICD-10 code can make the superbill incomplete, while using incorrect modifiers may change the meaning of a procedure or cause a denial.
✅ How to prevent:
- Double-check all diagnosis and procedure codes before submission.
- Use updated coding software or refer to AAPC’s coding guidelines.
- Implement a coding review step before claims are finalized.
Incorrect Patient or Insurance Details
If patient information (like date of birth or insurance ID) is wrong or incomplete, the claim may be rejected immediately by payers.
✅ How to prevent:
- Always verify patient demographics and insurance eligibility before creating the superbill.
- Encourage front-office staff to confirm updates at each visit.
- Maintain a standardized data entry checklist for all encounters.
Outdated CPT/ICD Codes
Medical coding systems are frequently updated. Using outdated codes can trigger claim rejections, compliance issues, or underpayments.
✅ How to prevent:
- Stay current with annual CPT and ICD-10 code changes.
- Schedule periodic coder training and compliance audits.
- Partner with certified medical coders who stay aligned with CMS updates.
Digital Superbills and EHR Integration
Modern healthcare practices are steadily shifting from paper-based superbills to digital superbills integrated within their Electronic Health Record (EHR) systems. This transition significantly simplifies superbill creation, submission, and tracking throughout the billing process.
EHR systems automatically pull patient demographics, diagnosis codes, and procedure details directly into the superbill template, reducing manual data entry errors. They also enable billing teams to track claim progress and identify issues early before submission. Automation further minimizes repetitive administrative tasks, ensuring each superbill in medical billing is complete, compliant, and ready for clean claim submission.
To explore how technology can improve your billing workflows and accuracy, check out our Tech Services page for tailored digital solutions.
Conclusion
Accurate superbills are the foundation of a successful revenue cycle. They connect clinical documentation to billing accuracy, ensuring every service is properly coded and reimbursed on time. By focusing on detail, automation, and regular audits, healthcare providers can eliminate costly claim errors and speed up payments. In today’s data-driven healthcare environment, a well-structured superbill in medical billing is no longer optional, it’s essential for financial efficiency and compliance.
Want to simplify your process? Talk to a Medical Billing Expert today and discover how professional billing support can transform your revenue cycle.
Frequently Asked Questions
A superbill typically includes patient demographics, provider details, procedure (CPT) and diagnosis (ICD-10) codes, date of service, and any modifiers or notes relevant to the visit.
A superbill is an internal document used by providers to communicate what services were performed. A claim form, like the CMS-1500, is the standardized format submitted to insurance payers for reimbursement.
Usually, the provider or clinical staff prepares the superbill after documenting the patient visit. The billing or coding team then reviews it for accuracy before claim submission.
Yes. Most EHR and practice management systems can automatically generate superbills based on clinical documentation, reducing manual entry and improving claim accuracy.