In medical billing, a clean claim means a claim submitted without errors, delays, or missing information. These claims get paid faster, reduce denials, and improve your practice’s cash flow. However, even minor errors, like a wrong patient ID or code mismatch, can slow payments. Understanding and fixing these issues helps your billing team ensure accuracy, consistency, and smoother reimbursement cycles.
Table of contents
What Is a Clean Claim and Why Does It Matter for Your Practice
A clean claim includes correct patient details, procedure codes, provider information, and necessary documentation. When payers receive a clean claim, they process it without asking for clarifications or resubmissions. This reduces administrative workload and supports steady revenue flow.
Maintaining clean claims ensures your billing team stays focused on growth rather than fixing avoidable issues. In later stages of the revenue cycle, even small errors can snowball into denials or cash flow problems, something no healthcare practice can afford.
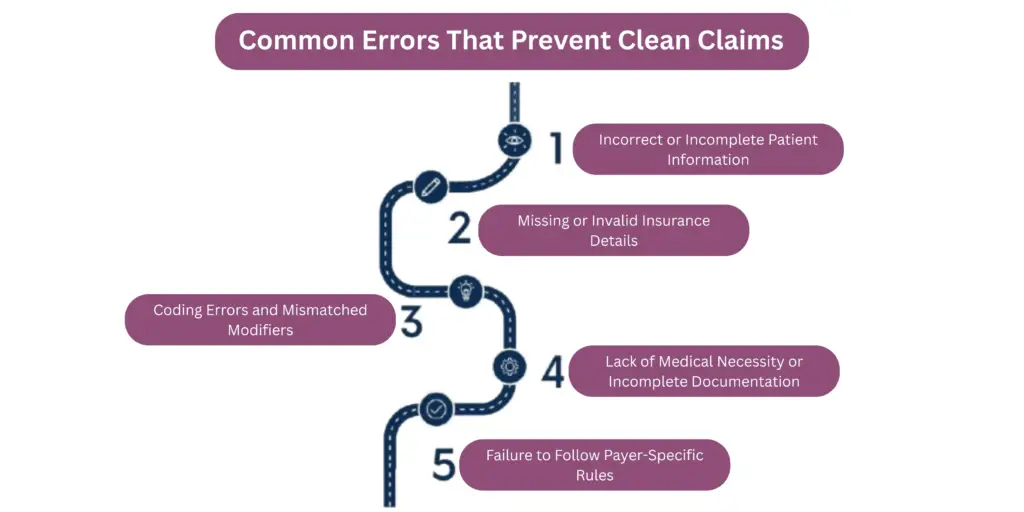
Common Errors That Prevent Clean Claims
Even the best billing systems can produce errors if small details slip through. Identifying and correcting these issues early helps ensure faster reimbursements and fewer denials. Below are the most common mistakes that prevent healthcare practices from submitting clean claims.
Incorrect or Incomplete Patient Information
Many claim denials start at registration. Errors in patient names, date of birth, or insurance ID can cause automatic rejections. Even a single typo can delay payments.
To avoid this, always verify patient data at each visit and ensure it matches payer records. Using real-time eligibility checks helps confirm coverage before services are rendered, keeping your claims accurate from the start.
Missing or Invalid Insurance Details
Outdated policy numbers or inactive plans are major reasons claims get rejected. Front desk teams often miss updates when patients change jobs or switch insurers.
Establish a consistent process for verifying insurance details before appointments. Encourage your staff to confirm coverage through payer portals or integrated verification tools. This small step ensures clean claims and reduces administrative rework later.
Coding Errors and Mismatched Modifiers
Accurate coding is the foundation of a clean claim. Incorrect CPT or ICD codes, or missing modifiers, can lead to costly rejections.
Regular audits and coder training sessions help prevent these issues. Partnering with a professional team like our Medical Coding Services ensures every procedure is billed correctly the first time.
Lack of Medical Necessity or Incomplete Documentation
Insurance payers require proof that each service is medically necessary. Missing notes, incomplete charting, or vague descriptions often trigger denials.
To fix this, encourage providers to document procedures clearly and consistently. Using electronic health records (EHR) templates and checklists helps standardize notes and maintain compliance, resulting in more clean claims.
Failure to Follow Payer-Specific Rules
Each insurance company has unique claim submission requirements. These may include specific documentation, pre-authorization codes, or filing timelines.
Billing teams that rely on outdated payer information risk unnecessary denials. Maintain an updated payer guideline list and review it quarterly. This proactive approach helps your team stay compliant and ensures each claim meets payer criteria.
How to Prevent Clean Claim Errors in Your Practice
Achieving a consistent rate of clean claims in medical billing requires more than accurate coding. It demands a combination of trained staff, automation, and continuous quality improvement. Implementing the right strategies not only reduces denials but also improves overall cash flow and operational efficiency.
Staff Training and Quality Checks
Your team plays a direct role in maintaining claim accuracy. Regular staff training helps billing specialists stay updated with payer policies, modifier rules, and medical coding standards.
Establishing internal quality audits ensures recurring errors are detected early. QA teams can review sample claims every week to identify patterns, correct errors, and provide targeted feedback. This proactive approach keeps your billing process compliant and efficient.
Automate Claims Scrubbing and Verification
Manual claim review can miss small but costly errors. Automated scrubbing tools and EHR-integrated systems flag inconsistencies in real time before submission. Tools aligned with HIPAA electronic claims standards enhance error detection, ensure compliance, and expedite payer approvals.
Automation helps verify patient data, insurance details, and code validity in seconds — significantly improving the clean claim rate.
Track Denials and Correct Upstream Processes
Even with preventive measures, some denials will still occur. The key is learning from them. By analyzing denial trends, billing managers can identify recurring issues such as incorrect codes, missing authorizations, or payer-specific rule violations.
Regular denial reports help teams correct upstream processes and prevent similar errors in the future. To streamline this step, explore our Denial Management solutions designed to resolve root causes and optimize claim accuracy.
Tools and Checklists for Clean Claims
Clean claim submission depends on teamwork, consistency, and the right use of technology. A structured checklist helps every department — from front desk to billing — stay aligned and accountable. Below is a simple reference table showing how each error type can be prevented with the right tool and team responsibility.
| Error Type | Prevention Tool | Responsible Team |
|---|---|---|
| Incomplete patient information | Real-time eligibility verification software | Front Desk / Registration |
| Invalid or outdated insurance details | Automated payer database and EHR integration | Billing / Verification Team |
| Coding errors or missing modifiers | Coding audit tool or EHR coding module | Coding Department |
| Missing documentation | Provider documentation checklist in EHR | Clinical Staff |
| Missed pre-authorization | Payer authorization tracking dashboard | Billing / Authorization Team |
| Denial trend repetition | Denial analytics and reporting tool | AR / Denial Management Team |
To make this process even easier, create a weekly clean claim checklist that ensures all claim fields are verified before submission.
💡 Tip: Offer the checklist as a downloadable document for staff. It becomes a quick reference guide to minimize claim errors and keep your cash flow strong.
Conclusion
Building a clean claim process is essential for consistent and timely reimbursements. Accuracy, proper documentation, and automation all play a critical role in avoiding errors that slow down payments. Regular staff training ensures that every claim meets payer requirements, while technology helps verify data before submission.
Clean claims in medical billing lead to faster approvals, reduced rework, and better cash flow for healthcare practices. By focusing on prevention, quality checks, and process improvement, your team can maintain a smooth revenue cycle and improve overall financial performance.
Talk to a Medical Billing Expert to learn how Practice Perfect can help you achieve higher claim accuracy and reliability.
Frequently Asked Questions
A clean claim contains complete and accurate information, submitted correctly on the first attempt so the payer can process it without delay.
Medical billing software automates data verification, checks coding accuracy, and alerts teams about missing information. This automation reduces manual errors and helps ensure that claims are clean before submission.
A rejected claim is returned before it enters processing due to errors like incorrect data or formatting. A denied claim is processed but not paid, usually because of policy exclusions or incomplete documentation.
Claims should be audited regularly, at least once a month, to identify trends and correct recurring issues. Routine audits help maintain compliance and improve the overall clean claim rate.