In medical billing, claim rejections are one of the most common roadblocks that disrupt the revenue cycle. Unlike denials, which occur after a claim is processed, rejections happen before the payer accepts the claim into their system. Understanding the different levels of rejection helps billing teams identify the root cause, apply targeted fixes, and prevent recurring issues. Each rejection level represents a unique problem within your billing workflow, from data entry mistakes to deeper compliance errors. By knowing these levels, practices can respond quickly, reduce rework, and maintain a smooth cash flow.
Table of contents
What Are the Levels of Rejection?
Medical billing rejections are generally categorized into three main levels, based on the nature and complexity of the issue. Identifying the right level ensures that claims are addressed correctly the first time, minimizing payment delays and administrative costs.
Level 1: Quick Fix / Resubmit Rejections
Level 1 rejections are usually minor, easily correctable issues that prevent a claim from being accepted by the payer’s system. These may include missing patient information, invalid insurance IDs, or simple formatting errors. Because the claim was never officially received, it can be corrected and resubmitted without going through a formal appeal.
Billing teams should have automated claim scrubbing tools and front-end validation processes to catch these errors before submission. Correcting Level 1 rejections promptly helps maintain cash flow and avoids unnecessary processing delays.
Level 2: Systemic Workflow or Process Rejections
Level 2 rejections indicate deeper, recurring issues that stem from workflow inefficiencies or procedural breakdowns. Common examples include incorrect use of CPT or ICD-10 codes, missing modifiers, or outdated payer requirements. These rejections often affect multiple claims or providers, signaling the need for process review, staff training, or software updates.
When Level 2 errors occur, practices must conduct root cause analysis to pinpoint where the process failed—whether during coding, charge entry, or claim submission. Resolving these at the system level significantly reduces future rejection rates.
Level 3: True Denials or Appeals-Required Rejections
Level 3 represents the most severe category, where the claim has been processed but denied for payment due to issues like lack of medical necessity, untimely filing, or missing documentation. Unlike Level 1 or Level 2, these require a formal appeal or reconsideration process with the payer.
Handling Level 3 rejections effectively demands in-depth payer knowledge, detailed documentation, and compliance expertise. These cases often require coordination between coders, billers, and clinicians to gather the necessary evidence for successful reimbursement.
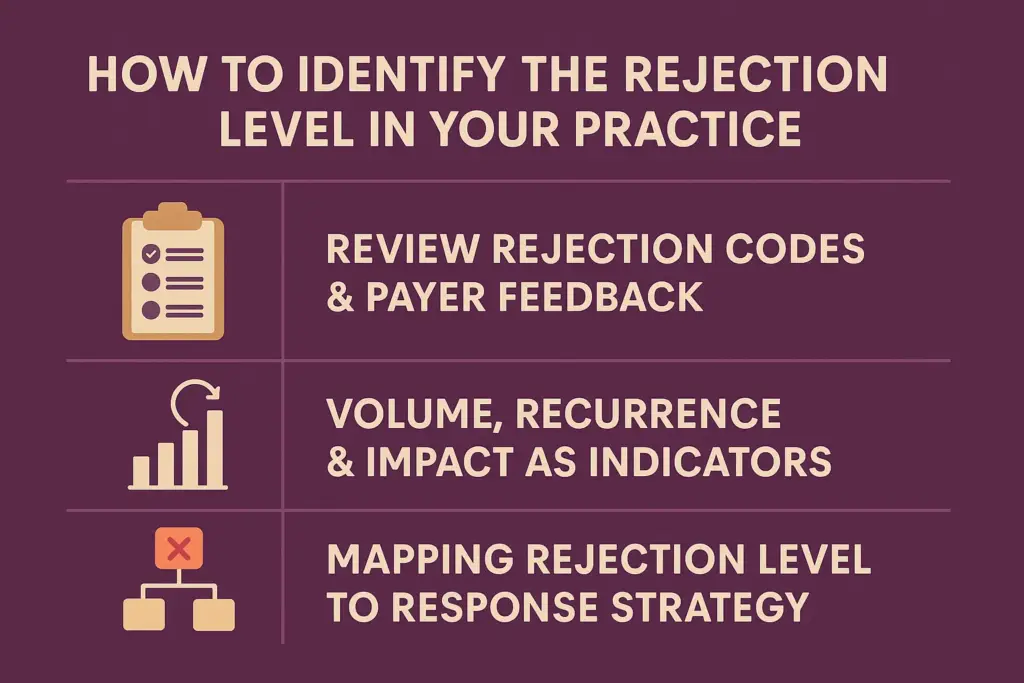
How to Identify the Rejection Level in Your Practice
Understanding why a claim was rejected starts with knowing what level of rejection it falls under. Identifying the rejection level helps your billing team determine whether the issue is a quick fix, a recurring workflow problem, or a denial that requires appeal. This structured approach minimizes confusion, improves turnaround times, and strengthens overall revenue performance.
Review Rejection Codes & Payer Feedback
Every payer provides specific rejection codes and messages that indicate the reason a claim was not accepted. These codes are your first clue in determining the rejection level. For example, if the code points to a missing field or invalid ID, it’s likely a Level 1 quick-fix rejection. If it highlights coding inconsistencies or documentation gaps, it may fall under Level 2 or Level 3.
Regularly reviewing electronic remittance advice (ERA) and clearinghouse reports ensures you don’t miss these signals. A proactive billing team should categorize these codes systematically within their billing software to flag recurring issues early.
Our Medical Billing Services include detailed rejection analysis and reporting to ensure every claim meets payer standards before submission.
Volume, Recurrence & Impact as Indicators
Tracking how often and where rejections occur can reveal valuable insights. High-volume or repeated rejections usually point to process-level issues (Level 2), such as incorrect templates or outdated payer rules. In contrast, isolated rejections tied to specific cases may reflect data entry or timing errors (Level 1).
By evaluating the frequency, recurrence, and financial impact, you can identify whether your practice needs staff retraining, improved front-end validation, or enhanced denial management tools. Consistent monitoring not only improves accuracy but also prevents costly bottlenecks in your revenue cycle.
Mapping Rejection Level to Response Strategy
Each rejection level demands a distinct response.
- Level 1: Correct and resubmit quickly, focusing on automation and front-end claim scrubbing.
- Level 2: Audit internal processes, retrain staff, and update payer-specific workflows.
- Level 3: Prepare detailed appeals with complete documentation and payer correspondence.
Establishing a clear escalation pathway ensures every team member knows how to handle rejections efficiently. Practices that integrate automated tracking systems and routine performance audits experience fewer delays and more consistent cash flow.
For further insights on reducing claim errors, check out our blog on Denial Prevention Strategies Every Practice Should Follow.
Why Each Level Requires a Different Response
Not all claim rejections are created equal, and neither should your response be. Each level of rejection reflects a different root cause, requiring a tailored strategy to prevent revenue delays. Addressing rejections correctly the first time improves claim acceptance rates, reduces rework, and enhances cash flow consistency.
Level 1 Response: Data Cleanup & Fast Resubmission
Level 1 rejections typically occur due to data entry mistakes or missing claim fields, issues that can be fixed and resubmitted quickly. Examples include incorrect patient IDs, outdated insurance details, or typos in CPT or ICD-10 codes.
At this level, speed and accuracy matter most. Implementing automated claim scrubbing tools and front-end verification during patient intake helps prevent simple mistakes before submission. Once corrected, these claims can often be resubmitted within hours, avoiding cash flow interruptions.
For consistent claim accuracy, explore our Insurance Verification Services to ensure every submission meets payer requirements from the start.
Level 2 Response: Process Redesign & Training
Level 2 rejections reveal systemic workflow gaps such as repeated coding errors, unclear internal procedures, or inconsistent documentation standards. These issues often demand process-level changes and staff retraining rather than one-time fixes.
Conducting internal audits, reviewing payer feedback patterns, and setting up training sessions for your billing and coding team can address recurring problems. Automated tracking tools also help identify where workflow failures originate — whether at scheduling, coding, or submission.
This level is where denial prevention and process optimization play a crucial role. Refer to our detailed blog on Top 10 Denials in Medical Billing to understand common triggers and preventive steps.
Level 3 Response: Appeal Management & Strategic Recovery
Level 3 rejections escalate into true denials, where payer adjudication requires appeals or formal reconsideration. These typically stem from medical necessity disputes, documentation insufficiencies, or missed deadlines.
Handling these rejections demands expertise in appeal documentation, payer communication, and timely follow-ups. Practices should maintain complete audit trails and standard appeal templates to ensure compliance. Strategic recovery teams can also track win rates and payer behavior to refine future submissions.
Common Causes Behind Each Rejection Level
Recognizing what triggers each rejection level is key to reducing their frequency. While many issues seem similar, the underlying causes differ based on where the claim fails in your billing workflow.
Front-End Issues: Eligibility, Demographics
Most Level 1 rejections arise before a claim even reaches the payer, often due to inaccurate patient information or insurance eligibility errors. Missing demographic details, outdated coverage, or invalid policy numbers lead to instant rejections.
Verifying insurance at every visit and keeping patient profiles updated in your EHR system prevents these errors. Routine front-end audits also help maintain data accuracy across departments.
Workflow Breakdowns: Coding, Documentation, Modifier Errors
Level 2 rejections emerge when claims repeatedly fail due to internal workflow inefficiencies. Common causes include incorrect coding combinations, missing modifiers, or inconsistent documentation between the provider and billing team.
Such issues require more than rework, they need process standardization and staff alignment. Regular quality checks, coding audits, and detailed documentation reviews can drastically reduce these rejections.
Medical Necessity, Timely Filing, Payer Policy Issues
Level 3 rejections or true denials occur when payers reject claims after adjudication due to lack of medical necessity, policy mismatches, or missed filing deadlines. These denials have the most financial impact since they require appeals and supporting evidence.
To prevent them, practices should stay updated with payer-specific rules, ensure all documentation supports medical necessity, and maintain a timely filing log. Regular staff training and compliance audits help ensure adherence to payer guidelines.
For authoritative updates, refer to resources like the AMA CPT Editorial Panel for coding compliance and policy changes.
How Practice Perfect Helps You Manage Rejections Efficiently
Handling rejections isn’t just about fixing errors, it’s about understanding why they happen and implementing systems that prevent them from recurring. That’s where Practice Perfect comes in.
Our team triages every rejected claim by rejection level, identifies the root cause, and applies targeted strategies to resolve and prevent similar issues. Whether it’s a Level 1 typo, a Level 2 workflow gap, or a Level 3 payer denial, we ensure your claims are corrected and resubmitted swiftly.
We combine expertise with automation to track claim patterns, streamline billing operations, and reduce manual workload. With dedicated teams focusing on front-end accuracy, compliance, and appeal management, we help practices recover lost revenue faster and sustain long-term financial stability. With Practice Perfect, your team gains clarity, control, and confidence from claim submission to reimbursement.
Final Thoughts
Understanding the levels of rejections in medical billing isn’t just a technical skill, it’s a financial strategy. By identifying whether a rejection stems from missing data, process gaps, or payer-specific issues, your team can take the right corrective action faster and protect revenue continuity. Efficient rejection management directly impacts your bottom line. When handled correctly, every rejection becomes an opportunity to strengthen your revenue cycle and reduce long-term denials.
Talk to a Medical Billing Expert today to streamline your rejection management and secure faster, cleaner reimbursements.
FAQs
A rejected claim does not make it through the payer’s processing system, often due to data or format errors. A denied claim is reviewed but not paid, usually because of eligibility, medical necessity, or policy issues.
If an issue occurs repeatedly due to process gaps, it’s Level 2. If it requires an appeal or payer intervention, it’s Level 3. Tracking rejection codes and response timelines helps identify the correct level.
Yes. If minor errors aren’t corrected promptly, they can miss timely filing deadlines and escalate into full denials. Quick action on Level 1 rejections prevents revenue loss.
Monitor metrics such as first-pass acceptance rate, rejection recurrence rate, appeal success rate, and average days to rework. These KPIs reveal where process improvements are most needed.