A healthy cash flow keeps every healthcare practice running smoothly. Yet many providers struggle with delayed payments and poor billing follow-ups. Effective billing collection strategies reduce revenue leaks, shorten AR cycles, and improve financial stability. By creating a structured process for claims, payments, and denials, practices can focus more on patient care and less on financial stress. At Practice Perfect, we help healthcare providers strengthen their cash flow through proven medical billing and collection solutions.
Table of contents
Why Billing and Collections Matter for Cash Flow
Strong billing and collection processes form the backbone of financial health in any medical practice. When payments get delayed, operational costs rise and revenue cycles slow down. Regular claim submissions, timely patient follow-ups, and accurate billing data improve your cash flow and reduce outstanding balances. A well-managed billing system ensures steady revenue, fewer denials, and higher patient satisfaction.
Our Revenue Cycle Management services can optimize your financial outcomes and maintain consistent cash flow.
Common Challenges in Healthcare Collections
Even with a structured billing process, many practices face common barriers that impact cash flow. Understanding these challenges helps identify weak spots in your revenue cycle and fix them early.
Patient Payment Delays and Communication Gaps
Patients often delay payments due to unclear bills, high out-of-pocket costs, or confusion about coverage. Transparent communication, digital payment options, and clear financial policies reduce these delays. Sending reminders through patient portals or text messages also improves collection rates. Training your front desk to explain payment expectations at check-in keeps balances under control.
Insurance Claim Denials and Rejections
Claim denials are one of the biggest causes of revenue loss in healthcare. Most denials occur because of missing data, eligibility issues, or incorrect codes. Tracking denial patterns helps your billing team prevent repeat errors. For expert support in minimizing claim rejections, Learn about Denial Management that focuses on quick identification and resolution.
Coding or Billing Errors
Incorrect procedure codes, mismatched modifiers, or incomplete documentation often delay reimbursements. Every claim must follow payer-specific rules to ensure clean submissions. Using reliable coding audits and staff training prevents such costly errors. Our Medical Coding Services help practices maintain coding accuracy and compliance for faster payment cycles.
Inefficient Follow-Up Processes
Many claims remain unpaid because staff fail to follow up consistently. Without timely reminders or AR tracking, overdue accounts pile up. Automating follow-ups and setting clear timelines improve collection success. Partnering with a professional AR Recovery team ensures every outstanding payment gets the attention it deserves.
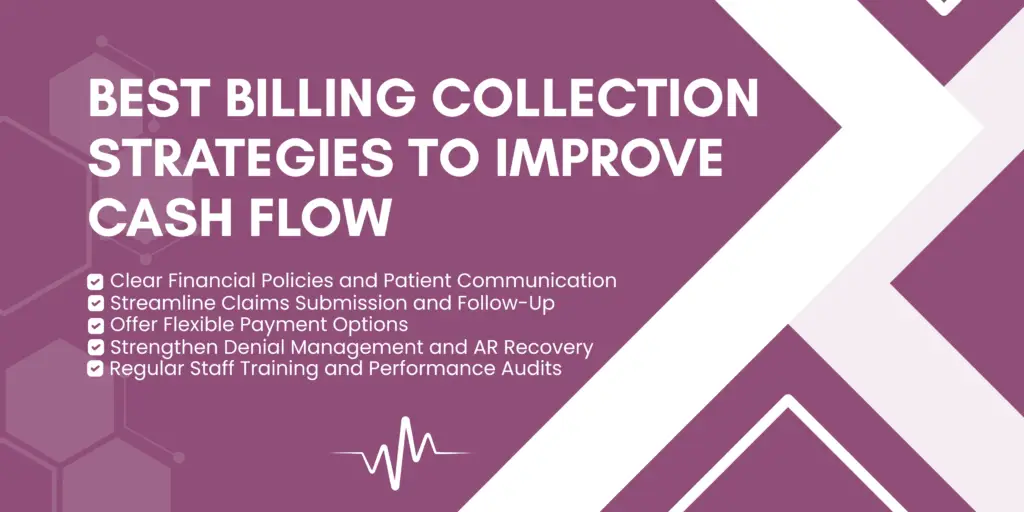
Best Billing Collection Strategies to Improve Cash Flow
Improving healthcare cash flow requires more than just timely billing. It’s about creating a streamlined, patient-friendly collection process that minimizes errors and accelerates reimbursements. Below are proven strategies that help your practice maintain financial stability and efficiency.
Clear Financial Policies and Patient Communication
A clear financial policy sets expectations from the start. Patients should understand their payment responsibilities before receiving care. Provide transparent cost estimates, insurance coverage details, and payment options during registration. Offering printed or digital copies of your financial policy ensures everyone stays informed, reducing confusion and payment delays.
Streamline Claims Submission and Follow-Up
A fast, error-free claim submission process speeds up reimbursements. Use automation tools to verify patient eligibility, submit claims electronically, and send follow-up reminders. Real-time tracking helps billing teams identify issues before they become denials. Efficient claim workflows not only improve cash flow but also reduce administrative workload.
Offer Flexible Payment Options
Patients are more likely to pay when it’s convenient. Offer flexible payment plans, credit card options, and secure online portals for quick transactions. Mobile-friendly payment systems simplify the process further. Providing multiple options supports better patient satisfaction while improving overall collection rates.
Strengthen Denial Management and AR Recovery
Effective denial management ensures every rejected or delayed claim gets resolved quickly. Identify recurring denial reasons and fix them at the source. A proactive Denial Management system reduces revenue leakage, while strong AR Recovery processes ensure older claims don’t go uncollected. Consistent tracking and timely follow-up are key to stable cash flow.
Regular Staff Training and Performance Audits
Billing and front-desk staff play a crucial role in collections. Regular training keeps them updated on coding rules, payer guidelines, and communication best practices. Monthly audits help identify process gaps and reinforce accountability. A knowledgeable team ensures accuracy, compliance, and faster revenue recovery.
Leveraging Technology for Faster Collections
Technology plays a vital role in improving cash flow and minimizing delays in the billing cycle. Automated systems, integrated tools, and real-time data help healthcare practices collect payments faster and reduce manual errors. Here’s how smart technology solutions can transform your collection process.
Practice Management Systems and EHR Integrations
A unified system connects billing, scheduling, and patient data for seamless communication. Integrating Electronic Health Records (EHR) with your practice management system ensures claims are accurate and complete before submission. This minimizes claim rejections and saves staff time spent on manual checks. Practices that use connected systems often see a noticeable boost in reimbursement speed.
Payment Automation Tools
Automated payment tools simplify how patients pay and how staff track transactions. These systems can send reminders, process payments instantly, and record receipts automatically. With fewer manual steps, your billing team can focus on strategic tasks like analyzing trends or improving patient communication. Automation also reduces human error and speeds up cash posting.
Real-Time Eligibility and Verification Tools
Eligibility verification tools confirm patient coverage instantly before the service is provided. This prevents claim denials due to invalid insurance or inactive policies. Real-time tools also help staff collect accurate copay or deductible amounts upfront, improving overall revenue consistency.
Technology Tools and Their Benefits for Collections
| Technology Tool | Benefit for Collections |
|---|---|
| EHR–Billing Integration | Fewer claim errors, faster submissions. |
| Automated Payment Systems | Instant payments, reduced manual workload. |
| Real-Time Eligibility Verification | Prevents coverage-related denials, ensures upfront payment accuracy. |
| Claim Tracking Dashboards | Improves visibility into pending or denied claims. |
| Reporting & Analytics Platforms | Identifies bottlenecks and improves financial forecasting. |
Outsourcing Collections to Experts
Outsourcing medical billing and collections can transform how a practice manages revenue. By partnering with professionals, healthcare providers reduce administrative burden and improve recovery rates. Trained billing teams handle complex denials, patient follow-ups, and aging claims efficiently, freeing your staff to focus on patient care.
Benefits of Outsourcing (Reduced AR, Higher Recovery Rates)
Expert billing partners use proven workflows and advanced tools to minimize errors and improve cash flow. Outsourcing helps practices reduce Accounts Receivable (AR) days, recover more from overdue claims, and prevent costly write-offs. With expert oversight, your revenue cycle becomes faster and more predictable.
KPIs to Track: AR Days, Collection Ratio, Patient Balance Trends
Tracking key performance indicators (KPIs) ensures transparency and continued improvement. Focus on:
- Average AR Days: Measures how long payments take to arrive.
- Net Collection Ratio: Evaluates how much of the collectible revenue is received.
- Patient Balance Trends: Shows how well your team manages patient payments.
When monitored consistently, these KPIs highlight areas to refine for stronger financial outcomes.
Want to enhance your billing performance? Talk to a Medical Billing Expert today and discover how outsourcing can help your practice achieve faster payments and better cash flow.
Conclusion
Efficient billing collection strategies play a critical role in maintaining a healthy cash flow. From transparent patient communication and real-time claim tracking to technology integration and outsourcing, every step contributes to better financial performance.
By optimizing internal processes, automating payment systems, and partnering with experts, practices can eliminate revenue delays and ensure stability. Start applying these strategies now to improve efficiency, reduce denials, and achieve consistent revenue growth.
FAQs
The most effective strategies include clear financial communication, automated reminders, real-time eligibility checks, and consistent denial follow-up.
Technology automates repetitive billing tasks, ensures accurate claims submission, and speeds up patient payments through online and mobile platforms.
Yes. Outsourcing helps reduce AR days, improve recovery rates, and minimize claim denials, resulting in a more consistent cash flow.
Focus on AR days, net collection ratio, denial rate, and patient balance trends to monitor financial performance effectively.