Submitting an appeal after a denied claim can feel like a second chance to recover lost revenue. But what happens when your claim appeals keep getting denied, too? This frustrating cycle costs your practice time, money, and productivity, often because of avoidable errors in the medical billing appeal process.
In this blog, we’ll break down the most common reasons appeals fail, and how to fix them to boost your approval rate and protect your revenue.
Table of contents
Why Do Claim Appeals Matter?
Every denied appeal represents delayed or lost income. According to the Centers for Medicare & Medicaid Services (CMS), nearly 1 in 5 claims is denied or delayed due to documentation or coding errors. For providers, this means more time spent chasing reimbursements instead of focusing on patient care.
Appeals are not just administrative tasks — they’re a safeguard for your financial stability. That’s why understanding the causes of repeated denials is essential.
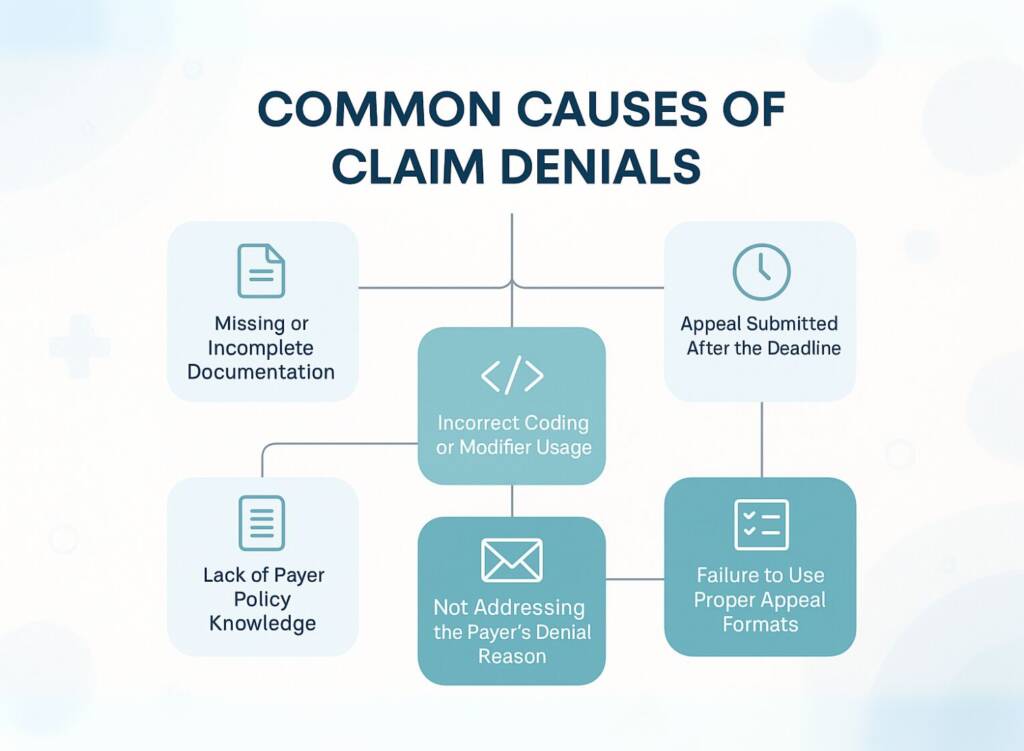
Common Causes of Claim Denials
Here are the common causes of Claim Denials:
Missing or Incomplete Documentation
One of the leading reasons appeals fail is missing documentation. Payers require detailed records such as:
- Operative or surgical reports
- Physician notes
- Diagnostic and lab results
- Prior authorization forms
Without these, insurers often reject appeals without review.
✅ Fix: Always attach every relevant record the first time you appeal. Implement a standardized documentation checklist for your billing staff to ensure nothing gets overlooked.
Incorrect Coding or Modifier Usage
Even if the denial reason seems unrelated to coding, errors in CPT, ICD-10, or modifier usage can trigger an automatic appeal rejection.
For example:
- Using the wrong ICD-10 diagnosis code for a procedure
- Omitting the modifier -25 when a significant E/M service is performed
- Linking codes incorrectly
✅ Fix: Review the original claim line-by-line for coding accuracy before resubmitting. Consider periodic coding audits to identify recurring mistakes.
Check Out how we ensure accurate medical coding services at Practice Perfect.
Appeal Submitted After the Deadline
Every payer enforces strict timelines for appeals, often 30–60 days from the denial notice. Missing this deadline usually results in an automatic rejection, regardless of merit.
✅ Fix: Use an automated denial tracking system to flag deadlines in advance. Assign accountability within your billing team to avoid missed opportunities.
Not Addressing the Payer’s Denial Reason
Another common mistake is resubmitting the same claim without addressing the insurer’s specific denial reason. Payers expect a point-by-point rebuttal.
For instance, if the denial reason is “medical necessity not established,” sending the same documents without additional clinical evidence won’t help.
✅ Fix: Carefully review the payer’s Explanation of Benefits (EOB) or denial code. Customize your appeal letter to directly counter the denial with supporting evidence.
Lack of Payer Policy Knowledge
Each payer has unique rules. Some require prior authorization, specific place of service (POS) codes, or certain documentation formats. Ignorance of these policies can lead to repeated denials.
✅ Fix: Maintain an updated database of payer-specific policies. Train your billing team quarterly to stay current with changes.
For more insights, check official payer guidelines at the American Medical Association (AMA).
Failure to Use Proper Appeal Formats
Insurance companies often require appeals to be submitted in specific formats — via designated forms, fax, or electronic portals. Using the wrong format can result in instant rejection.
✅ Fix: Before submission, verify the payer’s format requirements. Keep digital templates and appeal letters ready for each payer.
Common Causes of Appeal Denials & Solutions
| Cause of Denial | Impact | Solution |
|---|---|---|
| Missing documentation | Claim rejected without review | Use a checklist for all required documents |
| Incorrect coding/modifiers | Automatic appeal rejection | Conduct coding audits and reviews |
| Late submission | Appeal not reviewed | Implement denial tracking system |
| Ignoring denial reasons | Repeat rejections | Maintain an updated payer database |
| Lack of payer knowledge | Recurring denials | Verify requirements and use the correct forms/portals |
| Wrong format submission | Appeal rejected immediately | Implement a denial tracking system |
The Revenue Impact of Repeated Appeal Denials
Every denied appeal is not just lost income — it’s also wasted staff time and administrative resources. Over time, this can mean thousands of dollars in preventable revenue loss.
Practices that fail to optimize their appeal process often struggle with cash flow instability, making it harder to grow or reinvest in patient care.
How a Professional Billing Service Can Help
Outsourcing appeals to a professional medical billing service like Practice Perfect ensures your appeals are handled by experts who:
- Know payer-specific rules and compliance requirements
- Customize appeal letters to maximize approval chances
- Track deadlines and ensure timely submissions
- Conduct audits to prevent recurring denials
Explore our medical billing services to see how we help practices protect revenue.
Final Thoughts
Claim appeals don’t have to be a losing battle. By understanding the common causes of denial and addressing them proactively, your practice can improve appeal success rates, reduce wasted effort, and safeguard revenue.
If your staff is overwhelmed with repeated denials, outsourcing to experts is often the smartest step.
FAQs
It depends on the payer, but most appeals take 30–90 days for review and response.
Yes, some payers allow multiple levels of appeal, but requirements become stricter at each stage.
Industry studies suggest that about 35–45% of appeals succeed, higher when handled by experienced billing professionals.
Electronic submissions often process faster, but always follow the payer’s specific requirements.




