In medical billing, accuracy in coding is essential for ensuring smooth claim processing and timely reimbursements. Among the many medical code sets used by healthcare professionals, J codes hold a unique place. These alphanumeric codes are part of the HCPCS Level II system and are primarily used to identify drugs, biologics, and certain non-oral medications that cannot be self-administered. Understanding what J codes are and how they are applied helps healthcare practices prevent billing errors, reduce denials, and ensure proper reimbursement from payers.
Table of contents
What Are J Codes in Medical Billing?
J codes are specialized HCPCS (Healthcare Common Procedure Coding System) Level II codes used to report injectable drugs, chemotherapy agents, and biologics administered in a clinical setting. Each J code represents a specific medication and dosage, allowing payers to identify the exact treatment provided.
For example:
- J1100 – Injection, Dexamethasone Sodium Phosphate, 1 mg
- J1170 – Injection, Hydromorphone, up to 4 mg
- J3490 – Unclassified drugs (used when no specific J code exists)
J codes are essential for billing medications that are administered by injection or infusion, such as those given by a physician or nurse. They also play a critical role in tracking drug utilization, supporting compliance with payer policies, and ensuring accurate reimbursement rates under Medicare and commercial insurance plans.
Example: When a patient receives an injection during an office visit, the medical bill must include both the CPT code for the administration procedure and the J code for the drug itself. Missing or incorrect J codes can lead to claim rejections or underpayments.
Structure & Format of J Codes
Every J code in medical billing follows a consistent alphanumeric structure that starts with the letter “J” followed by four digits (e.g., Jxxxx). This format is part of the HCPCS Level II system and helps identify injectable medications and non-oral drugs used in patient treatment.
The “J” prefix instantly signals that the code belongs to the drug and biological products category, making it easier for billers and payers to recognize its purpose during claim submission.
Example of a J Code
A clear example of a J code is J1885, which represents:
J1885 – Ketorolac tromethamine, injection, 15 mg
This code is used to report the administration of Ketorolac, a nonsteroidal anti-inflammatory drug (NSAID) used for short-term pain management. Using the correct J code ensures that both the medication and the dosage are clearly documented, leading to faster claim processing and accurate reimbursement.
Units and Dosage Reporting
Each J code corresponds to a specific unit of measure, such as milligrams (mg), milliliters (mL), or international units (IU). When billing, healthcare providers must accurately record the number of units administered to ensure the claim reflects the true dosage.
For example, if a drug is billed as “per 10 mg” and the provider administers 30 mg, the claim should list three units for that J code. Incorrect unit reporting often leads to underpayment, claim rejections, or payer audits.
Partnering with professionals who understand these details can prevent costly mistakes. Learn more in our Revenue Cycle Management Services page to see how accurate billing and coding improve your reimbursement outcomes.
CMS and HCPCS Updates
The Centers for Medicare & Medicaid Services (CMS) regularly reviews and updates the HCPCS Level II code set, including J codes. These updates ensure that new drugs, dosage changes, and discontinued products are accurately represented in medical billing.
CMS releases these updates on a quarterly and annual basis, and billing teams need to stay informed. Using outdated codes can result in denied claims or delayed payments.
Commonly Used J Codes in Healthcare
The following table lists some of the most frequently used J codes in healthcare settings. These codes cover a wide range of medications, from pain relief to emergency treatments and oncology drugs.
| J Code | Drug / Service Description | Use Case Example |
|---|---|---|
| J1885 | Ketorolac Tromethamine | Pain management injection |
| J1100 | Dexamethasone | Anti-inflammatory injection |
| J0120 | Tetracycline | Antibiotic injection |
| J0171 | Adrenalin (Epinephrine) | Emergency allergy reaction |
| J9299 | Nivolumab | Oncology treatment |
This table provides a quick reference for common medications billed using J codes and helps ensure precise documentation during the claim process.
👉 You can read more about Modifiers in Medical Billing: A Complete Guide for Providers
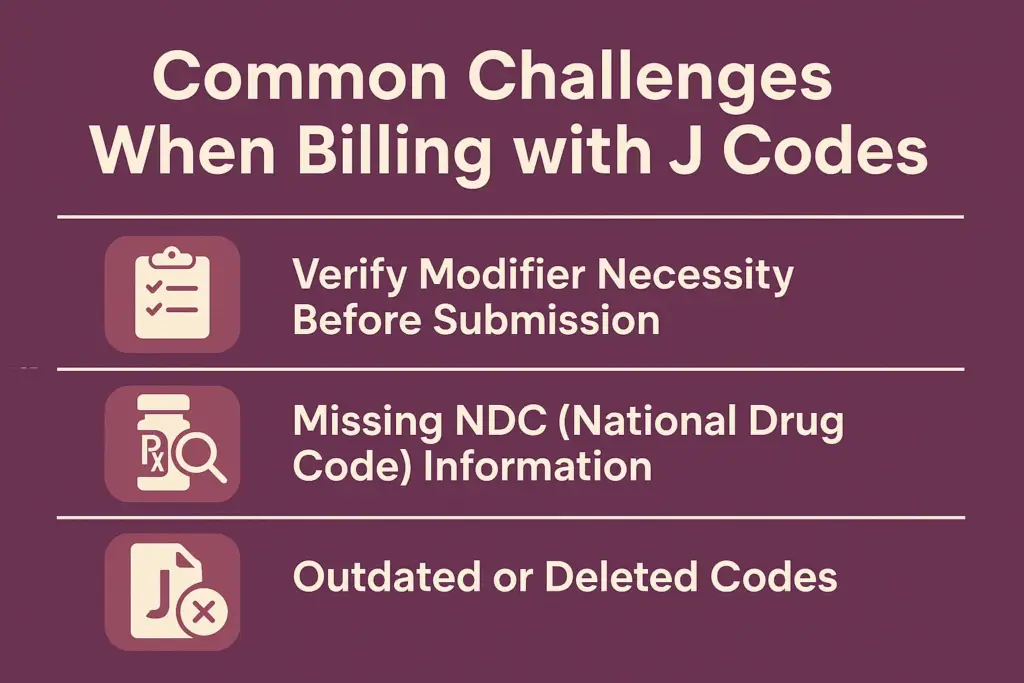
Common Challenges When Billing with J Codes
While J codes simplify drug billing, even small errors can cause claim denials or payment delays. Understanding common challenges helps practices prevent rejections and maintain clean claim submissions.
Incorrect Units or Dosage Reporting
One of the most frequent J code billing errors involves reporting incorrect units or dosage amounts. Since each J code represents a specific quantity (e.g., 10 mg, 1 mL, etc.), even minor mistakes can lead to underpayment or overbilling.
For example, if a provider administers 30 mg of a drug but bills only one unit instead of three, the claim reimburses for less than what was provided. These dosage errors often arise from poor documentation or a lack of coordination between clinical and billing teams.
Maintaining accurate dosage tracking is critical to ensure fair and timely reimbursement for administered drugs.
Missing NDC (National Drug Code) Information
Many payers now require that each J code be paired with a corresponding National Drug Code (NDC). The NDC identifies the drug’s manufacturer, formulation, and package size, ensuring precise billing transparency.
If the NDC is missing or mismatched, the payer may deny the claim or request additional documentation. This not only delays payment but also adds administrative burden to your billing team.
To prevent this, practices should always cross-check J codes and NDCs during claim preparation to ensure compliance and clean submissions.
Outdated or Deleted Codes
Using expired or outdated J codes is another common source of claim denials. The HCPCS Level II code set is updated regularly, with old codes deleted and new ones added to reflect current medical use.
Billing teams that rely on outdated code lists risk submitting invalid claims, which can delay cash flow and create compliance issues. Staying updated through official sources like CMS and professional organizations helps avoid such problems.
To ensure accuracy, work with experts who monitor every change in payer requirements. Learn more about our Medical Billing Services and how we help providers maintain coding accuracy.
Best Practices for Accurate J Code Billing
Following best practices for J code billing helps providers avoid denials, reduce administrative costs, and ensure compliance with payer policies.
Verify Drug Details and NDC Before Submission
Before submitting a claim, always verify the drug’s name, dosage, strength, and NDC. This ensures consistency between the clinical documentation and the billing system. Verifying this data minimizes payer rejections and supports clean, compliant claims.
Keep Drug Inventory and Billing Teams Aligned
Billing accuracy depends on strong communication between the pharmacy, clinical, and billing departments. Any changes in drug stock, formulation, or vendor should be immediately shared with billing teams. This alignment reduces errors caused by mismatched data or missing codes.
Use Software Tools for J Code Validation
Modern billing software can automatically validate J codes, NDCs, and dosage units before submission. These tools detect discrepancies early, preventing denials and saving time on rework.
Regularly Review CMS Updates
Since CMS updates J codes quarterly, billing teams need to review the latest updates and educate staff accordingly. Outdated codes are a leading cause of claim rejection, so routine code audits and staff refreshers are vital.
For more actionable tips, read our blog Denial Prevention Strategies Every Practice Should Follow. Staying informed and proactive is the best way to maintain clean claim submissions.
How Practice Perfect Ensures Clean J Code Billing
J code billing demands accuracy, compliance, and consistent updates — all of which can be challenging for in-house billing teams. At Practice Perfect, we specialize in simplifying this complexity by ensuring every claim meets payer and CMS standards.
Our billing experts follow a structured process to ensure clean claim submission and faster reimbursements:
- Code Validation & Compliance Checks
Every J code is reviewed against current HCPCS and CMS rules to prevent outdated or mismatched entries. - Integrated Verification Process
Our Insurance Verification Services confirm coverage details, reducing denials caused by missing or invalid payer data. - Comprehensive Claim Audits
We conduct internal audits to identify recurring J code issues, dosage inconsistencies, and documentation gaps before submission. - End-to-End Revenue Oversight
With our Revenue Cycle Management (RCM) and Medical Billing Services, we optimize the entire billing workflow — from code entry to final payment — ensuring complete accuracy and payer compliance.
By combining automation, experienced coders, and proactive audits, Practice Perfect helps providers eliminate rejections, speed up payments, and maintain revenue integrity.
Conclusion
J codes are vital to accurate medication billing and transparent reimbursement in modern healthcare. However, keeping up with dosage details, payer updates, and NDC requirements can be overwhelming for internal teams. Outsourcing to a specialized partner like Practice Perfect allows providers to focus on patient care while we handle the coding accuracy, compliance tracking, and claim follow-ups.
Frequently Asked Questions
J codes are used to identify injectable drugs, biologics, and some non-oral medications for reimbursement under HCPCS Level II. They allow payers to track the exact drug administered and ensure accurate payment.
While CPT codes describe procedures and services, J codes specifically represent medications and injections supplied during treatment. They often appear together on a claim — the CPT code for the service and the J code for the drug used.
Most Medicare and commercial payers require J codes for billing injectable or infused drugs. However, not all drugs have an assigned J code; in such cases, temporary or unclassified codes (e.g., J3490) may be used.
Billing teams should ensure accurate dosage entry, correct NDC pairing, and up-to-date HCPCS code usage. Regular training, system updates, and claim validation tools also help reduce J code-related denials.




